Research Forum
Thinning or loss of the outer third of the eyebrows is a sign of Poison/"Vitamin A" toxicity
Quote from Dr. Garrett Smith on March 20, 2019, 4:03 pmA thinning or loss of the outer third of the eyebrows is also known as the Sign of Hertoghe or Queen Anne's sign. This problem is normally stated all over the Wild West of the internet medical experts to be associated with low thyroid issues. Here's what I can tell you. We are seeing in clients who have been doing the Poison/"Vitamin A" and Glyphosate Detox Program that the outer/lateral third of their eyebrows are returning over time. How is this connected, you wonder?
Well, you might want to check my Poison/"Vitamin A" as the culprit behind nearly all our modern thyroid issues, as well as see the YouTube testimonial to the Poison/"Vitamin A" and Glyphosate Detox Program normalizing thyroid antibodies (as in, Hashimoto's autoimmune thyroid being resolved). Now, I'd like to present a case study of a man who self-poisoned himself with Poison/"Vitamin A" supplements (both carotenoids and retinoids), and when he STOPPED them, over a period of months, his lateral third of the eyebrows GREW BACK. I try to make these connections as obvious as possible, and they don't get any more obvious than this. Also, this is yet another example of how Poison/"Vitamin A" is also behind the "high triglycerides" and "high cholesterol" epidemics.
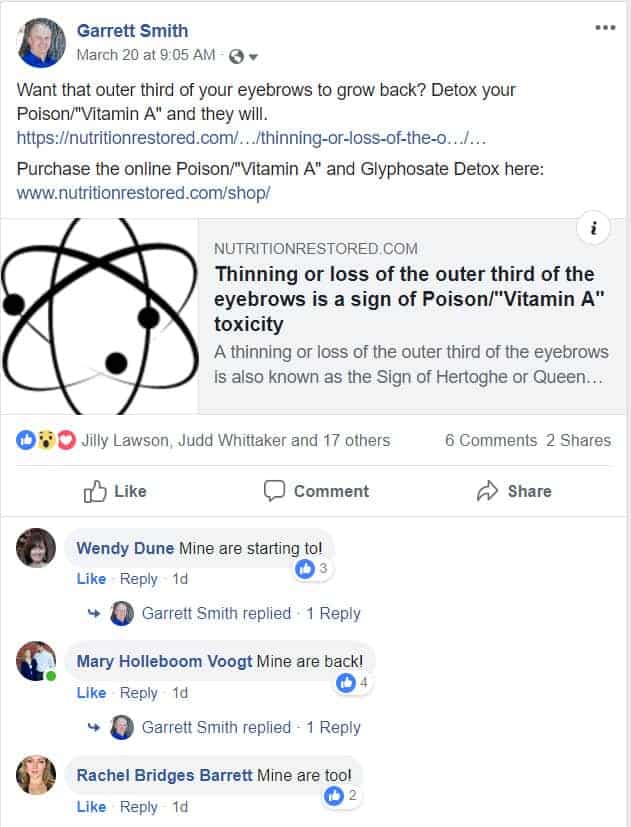
As the "proof is in the pudding", let me start by showing some people saying that by following my Poison/"Vitamin A" and Glyphosate Detox Program is allowing their lateral eyebrows to grow back in (note: all my FaceBook posts are public, so these comments were public as well):
Now that you have seen real-life evidence that this works, let's go into the scientific literature.
Hypervitaminosis A altering the lipid profile in a hypercholesterolemic patient(2009)
Erratic and supraphysiologic intake of vitamin A can lead to adverse effects that can be life threatening. For this reason, various medical societies have limited the recommended daily allowances and intakes (RDA and RDI, respectively) in an attempt to prevent hypervitaminosis toxicity. Studies have reported an association between hypertriglyceridemia and hypervitaminosis A. 2–4 We present a patient with a history of familial combined hypercholesterolemia who developed an abrupt increase in his total cholesterol (TC), low-density lipoprotein (LDL), and triglycerides (TG) after taking high doses of vitamin A supplements.[...]Case studyA 56-year-old Caucasian male who is an active mountain climber, presented to The Center for Heart Disease Prevention seeking medical advice regarding a recent abnormal lipid profile. At the time of his visit he had normal liver, thyroid and cortisol function tests and denied any headaches, visual changes, abdominal pain, or skin changes. He did not drink alcohol; was a nonsmoker; did not have a family history of coronary artery disease, dyslipidemia, or liver disease; and denied use of illicit drugs. He reported attempting to follow a healthy lifestyle and diet. In 1999, the patient was placed on 20 mg/day atorvastatin by his primary care physician, which was increased to 40 mg/day in 2001. He routinely checked his lipid profile every 6 months with his primary care physician. The lipid profile prior to the intake of vitamin A supplements revealed a TC of 204 mg/dL, LDL of 78 mg/dL, high-density lipoprotein (HDL) of 50 mg/dL and TG of 265 mg/dL. In March 2005, the patient started taking various vitamin supplements, including vitamin A, and recently had been taking extra doses of vitamin A supplements. The total daily intake included 8000 IU of vitamin A and 3500 IU of vitamin A included in a multivitamin tablet. He also consumed tablets reportedly containing 25,000 IU of beta-carotene. The patient took no other medications except the statin and the vitamin supplements. Subsequently, the patient’s lipid levels began to increase, peaking in February 2006 to TC, TG, and LDL levels of 780, 923, and 530 mg/dL, respectively. This was treated with the addition of fenofibrate 145 mg to atorvastatin 40 mg/day. In March 2006, the patient’s wife noticed thinning of the lateral eyebrows, suspected that this might be secondary to vitamin A toxicity, and asked her husband to discontinue these supplements. The supplements were stopped in March 2006, which coincided with a decrease in TC, TG, and LDL levels. Fenofibrate was discontinued and the patient was started on rosuvastatin in November 2007. A year after stopping the vitamin A supplements, his lipid profile had returned to the values recorded during atorvastatin therapy alone (Fig. 1). Over several months, his eyebrows returned to their normal state.
[...]
Our patient was treated for dyslipidemia that was well controlled prior to starting the daily intake of vitamin A supplements. The dramatic increase in the lipid profile resolved after discontinuation of the vitamin A supplements.ConclusionDaily intake of vitamin A in excess of the recommended RDA doses is discouraged.I wanted to interject here and remind you that the RDA for Poison/"Vitamin A" is 4000 IU for adult women, and 5000 IU for adult men, and that is the TOTAL from all sources, including foods, supplements, topically applied skincare...all of it. Many of you reading this may get this much in your multivitamin by itself, or even just your breakfast. That is a very low amount for people who are either "health seekers" and pushing high Poison/"Vitamin A" foods, or others who have no idea how to avoid it.
Large doses may prove particularly problematic in patients with dyslipidemia. This case is the first to document an association of the intake of very high doses of over-the-counter vitamin A supplements with marked dyslipidemia. In this case, apparent complete remission was achieved by discontinuing these supplements.
A thinning or loss of the outer third of the eyebrows is also known as the Sign of Hertoghe or Queen Anne's sign. This problem is normally stated all over the Wild West of the internet medical experts to be associated with low thyroid issues. Here's what I can tell you. We are seeing in clients who have been doing the Poison/"Vitamin A" and Glyphosate Detox Program that the outer/lateral third of their eyebrows are returning over time. How is this connected, you wonder?
Well, you might want to check my Poison/"Vitamin A" as the culprit behind nearly all our modern thyroid issues, as well as see the YouTube testimonial to the Poison/"Vitamin A" and Glyphosate Detox Program normalizing thyroid antibodies (as in, Hashimoto's autoimmune thyroid being resolved). Now, I'd like to present a case study of a man who self-poisoned himself with Poison/"Vitamin A" supplements (both carotenoids and retinoids), and when he STOPPED them, over a period of months, his lateral third of the eyebrows GREW BACK. I try to make these connections as obvious as possible, and they don't get any more obvious than this. Also, this is yet another example of how Poison/"Vitamin A" is also behind the "high triglycerides" and "high cholesterol" epidemics.
As the "proof is in the pudding", let me start by showing some people saying that by following my Poison/"Vitamin A" and Glyphosate Detox Program is allowing their lateral eyebrows to grow back in (note: all my FaceBook posts are public, so these comments were public as well):
Now that you have seen real-life evidence that this works, let's go into the scientific literature.
Hypervitaminosis A altering the lipid profile in a hypercholesterolemic patient(2009)
Erratic and supraphysiologic intake of vitamin A can lead to adverse effects that can be life threatening. For this reason, various medical societies have limited the recommended daily allowances and intakes (RDA and RDI, respectively) in an attempt to prevent hypervitaminosis toxicity. Studies have reported an association between hypertriglyceridemia and hypervitaminosis A. 2–4 We present a patient with a history of familial combined hypercholesterolemia who developed an abrupt increase in his total cholesterol (TC), low-density lipoprotein (LDL), and triglycerides (TG) after taking high doses of vitamin A supplements.[...]Case studyA 56-year-old Caucasian male who is an active mountain climber, presented to The Center for Heart Disease Prevention seeking medical advice regarding a recent abnormal lipid profile. At the time of his visit he had normal liver, thyroid and cortisol function tests and denied any headaches, visual changes, abdominal pain, or skin changes. He did not drink alcohol; was a nonsmoker; did not have a family history of coronary artery disease, dyslipidemia, or liver disease; and denied use of illicit drugs. He reported attempting to follow a healthy lifestyle and diet. In 1999, the patient was placed on 20 mg/day atorvastatin by his primary care physician, which was increased to 40 mg/day in 2001. He routinely checked his lipid profile every 6 months with his primary care physician. The lipid profile prior to the intake of vitamin A supplements revealed a TC of 204 mg/dL, LDL of 78 mg/dL, high-density lipoprotein (HDL) of 50 mg/dL and TG of 265 mg/dL. In March 2005, the patient started taking various vitamin supplements, including vitamin A, and recently had been taking extra doses of vitamin A supplements. The total daily intake included 8000 IU of vitamin A and 3500 IU of vitamin A included in a multivitamin tablet. He also consumed tablets reportedly containing 25,000 IU of beta-carotene. The patient took no other medications except the statin and the vitamin supplements. Subsequently, the patient’s lipid levels began to increase, peaking in February 2006 to TC, TG, and LDL levels of 780, 923, and 530 mg/dL, respectively. This was treated with the addition of fenofibrate 145 mg to atorvastatin 40 mg/day. In March 2006, the patient’s wife noticed thinning of the lateral eyebrows, suspected that this might be secondary to vitamin A toxicity, and asked her husband to discontinue these supplements. The supplements were stopped in March 2006, which coincided with a decrease in TC, TG, and LDL levels. Fenofibrate was discontinued and the patient was started on rosuvastatin in November 2007. A year after stopping the vitamin A supplements, his lipid profile had returned to the values recorded during atorvastatin therapy alone (Fig. 1). Over several months, his eyebrows returned to their normal state.
[...]
Our patient was treated for dyslipidemia that was well controlled prior to starting the daily intake of vitamin A supplements. The dramatic increase in the lipid profile resolved after discontinuation of the vitamin A supplements.ConclusionDaily intake of vitamin A in excess of the recommended RDA doses is discouraged.
I wanted to interject here and remind you that the RDA for Poison/"Vitamin A" is 4000 IU for adult women, and 5000 IU for adult men, and that is the TOTAL from all sources, including foods, supplements, topically applied skincare...all of it. Many of you reading this may get this much in your multivitamin by itself, or even just your breakfast. That is a very low amount for people who are either "health seekers" and pushing high Poison/"Vitamin A" foods, or others who have no idea how to avoid it.
Large doses may prove particularly problematic in patients with dyslipidemia. This case is the first to document an association of the intake of very high doses of over-the-counter vitamin A supplements with marked dyslipidemia. In this case, apparent complete remission was achieved by discontinuing these supplements.
Licensed Naturopathic Physician (NMD) in Arizona
NutritionDetective.com, home of the Love Your Liver program
YouTube - FaceBook - Instagram - Twitter
