Research Forum
Chris Masterjohn, a case study in chronic Vitamin A toxicity and thiamine deficiency
Quote from Dr. Garrett Smith on December 3, 2019, 12:58 amhttps://youtu.be/S8Jn86UaFPc
First, I would like to make people aware that my intention is to help Chris so that he can potentially fix his numerous health issues, and if that is not possible, I'm hoping to help the other people who read this article and/or watch the video. While myself and others in the crowd who have fully realized the poison that is the non-"Vitamin" A, Chris has previously taken to ad hominem character attacks on us when we brought it up, calling us things like "flat earthers". He particularly didn't care for when I linked his aggressive FaceBook replies to this paper discussing aggression and chronic Vitamin A toxicity. Others noted that any discussion of chronic Vitamin A toxicity on his FaceBook page was quickly deleted. Oh well.
I am not digging into his health history any more than what he has put on the internet himself. This post that he put on FaceBook about his recent health issues and adventures in the conventional medical system is the one I will be discussing. I've heard from others about his internet-admitted past issues with exercise intolerance, heat intolerance, and allergies...all things that we regularly see improve on the Vitamin A Detox Program.
Just in case that post were to disappear, and for those who refuse to create FaceBook accounts (I admire you), here are screenshots of the post:
There is no good reason to downplay any of the signs and symptoms showing up in the above. He is far too young to be showing these significant neurological symptoms...unless he potentially was becoming toxic with something, and/or was severely deficient in something else. There is evidence and arguments for both, as you will see, and both go together.
In this article, I will lay out the science that shows that Chris has a severe and worsening chronic Vitamin A toxicity problem, severe B-vitamin (particularly thiamine) deficiency problems, and that both of those issues are being exacerbated by continued alcohol consumption.
I'm not going to re-post any of the post's associated pictures, as I think the words above are enough. I did note that in two of the three associated pictures he posted he was holding a beer, and in this post he talks about four drinks in one night while the picture is of yet another beer. I don't care how much someone drinks, I only care about how it affects the body-system and plays into the clues that his case left for me, the "Nutrition Detective". You'll see the reason for that term as we go through this piece by piece. Important things to keep in mind as we go on from this part are that alcohol has extremely negative interactions with Vitamin A, and that alcohol depletes thiamine (Vitamin B1). We will cover those more below.
Chris Masterjohn is well-known in nutritional circles as being a superfan of the Weston A. Price Foundation's (WAPF) general dietary guidelines of consuming MASSIVE amounts of Vitamin A from foods (liver, eggs, dairy, cod liver oil, squashes, etc.) and incorrectly believing that food-based Vitamin A is somehow magickally, completely, and utterly non-toxic. How wrong they are, and their followers (who often become my clients trying to fix the damage) and their children pay the price for it.
It should also be known that on his website he promotes discounts--and thus likely has financial arrangements with--at least two companies that sell organ meats in various forms. Why is this important? The old saying, "It is difficult to get a man to understand something, when his salary depends upon his not understanding it!" applies here.
Here are some of his articles over at the WAPF website showing an extreme pro-Vitamin A bias:
Vitamin A On Trial: Does Vitamin A Cause Osteoporosis?
- One can get a real feel for his position of downplaying chronic Vitamin A toxicity from the title of this section: How Much Vitamin A is Too Much? The Wrong Question to Ask [NOTE: asking how much is TOO MUCH is the MOST IMPORTANT question to ask!!!]
Who can forget the article & video he did about how he somehow got "Vitamin A deficient" in less than one month, which is IMPOSSIBLE for anyone to do! How do I know this? First, with his assumed/implied Vitamin A-heavy diet, he is nowhere near deficient in Vitamin A. Vitamin A is fat-soluble, which means it is stored in the liver and all over the body. Medscape says: "An adult liver can store up to a year's reserve of vitamin A." He absolutely did not "get deficient" in one month of eating a "low-Vitamin A" diet, certainly not when he regularly eats as many Vitamin A foods as he does! What likely happened is that his body started DETOXING/DUMPING that poison, causing him detoxification symptoms, because it FINALLY had the opportunity to do so!
PRO TIP: Read the comments of that article, where multiple people are asking him about their own Vitamin A toxicity problems!
What if we had insight into his diet, straight from Chris himself? We do, it is here: Why a Carnivore Diet is Problematic With Dr. Chris Masterjohn
I'm only going to include the pertinent Vitamin A toxicity-inducing portions below.
Excerpts from the section "Chris’ Guide To The Ideal Diet":
- Diversify your source of protein (meat, fish, poultry, shellfish, eggs, dairy, etc.)
- Diversity within the animal
- Make an effort to eat nose-to-tail
- Add 4-8 oz of liver to your diet each week
- Replace some meat with heart (if you’re feeling more adventurous, try kidney)
- Consume a large volume of vegetables
- Several cups per day
- Diversify across the colors (green, red, orange, yellow)
Every item I bolded above is a significant source of Vitamin A. I go over this more in the video. In combination, it is a recipe for excess, as you shall see.
Excerpts from the section "Chris' Masterjohn's Actual Diet"
- Modified due to digestive issues and not being able to absorb fructose well
- Chris’ typical meal:
- White rice
- A lot of mixed vegetables
- Meat or eggs
- A tomato product (usually salsa)
- 1 tbsp of unfortified nutritional yeast
- Chris will take oyster extract and liver supplements throughout the day
- His main fruit is bell pepper and tries to eat all colors
I'm going to spend a bit of time on this part. Again, every part I bolded is either high in Vitamin A or aggravates Vitamin A toxicity (again, I cover this more in the video).
Note the part about "not being able to metabolize fructose well." Research has shown in rats that Vitamin A toxicity slows down a key enzyme directly involved in FRUCTOSE metabolism: Early effects of hypervitaminosis A on gluconeogenic activity and amino acid metabolizing enzymes of rat liver.
Furthermore, hypervitaminosis A decreased the activities of two key hepatic glycolytic enzymes, phosphofructokinase, and pyruvate kinase, without affecting those of hexokinase and glucokinase.
Probably not a coincidence.
Liver pills and oyster extract are concentrated sources of Vitamin A.
Tomatoes and bell peppers, along with their inflammatory nightshade nature (you might recognize the author of that blog post 😉 ), are both very high in carotenoid Vitamin A.
Vegetables in the red, yellow, and orange color spectrums will always be high sources of Vitamin A.
Here's the kicker though. A study from the 1950s showed that rats that were given yeast or any fraction of liver (water-soluble OR fat-soluble) along with Vitamin A, got much worse symptoms of Vitamin A toxicity than rats that only got Vitamin A. It is also of note that tuna solubles, fish solubles, and acetone-extracted herring roe also worsened the Vitamin A toxicity problems...so the oyster extract potentially is looking similar in effect.
Chris says that this is his regular daily diet. Extremely high in Vitamin A, along with 2, maybe 3, other factors in it that have been shown to worsen Vitamin A toxicity symptoms.
Now, let's go into his FB post. The quotes are from his post, my comments are in between.
I went in for an MRI last night. I was nervous AF about getting injected with gadolinium contrast and you can probably tell the anxiety level is way higher in my before picture versus in the post-MRI beer pic.
I want to get to the bigger things first. I re-visit the anxiety below, after painting the bigger picture first.
I’m investigating an abnormal gait that has crept up on me three times now.
A recurring/repeating issue could easily imply that either a toxicity state keeps returning, or a deficiency state keeps returning, or both. One should be able to figure out that if it is recurring, the root cause of the problem has NOT been dealt with. It has only been symptomatically addressed.
Is "abnormal gait" a symptom of chronic Vitamin A toxicity? Yes, and across multiple species.
In cats: Skeletal Abnormalities in the Hindlimbs of Young Cats as a result of Hypervitaminosis A
HYPERVITAMINOSIS A causes extensive confluent exostosis formation of the cervical spine in adult cats1,2. It was initially reported that no juvenile osteodystrophy occurred in this disease1, but an abnormal hindquarter gait was described later in a group of young cats receiving large daily doses of vitamin A (ref. 2). No explanation of this abnormal gait was given and the condition was therefore studied further.
Add in pigs and humans: Hypervitaminosis A in the pig.
Premature cIosure of epiphyseal cartilages and changes in the structure of epiphyses themselves, gave rise to joints of abnormal structure, direction and amplitude of movement leading to lameness and gait changes. This has been amply demonstrated in experimental hypervitaminosis A of young cats (Clark and Seawright 1968) and also in children recovering from hypervitaminosis A (Pease 1962).
"...amply demonstrated..." I think that is strong enough wording from a 50-year-old paper for my purposes here.
Now, let's move on to thiamine. Has thiamine deficiency ever been associated with "abnormal gait"? Yes. So much so that there's a specific name for the neurological triad of disease symptoms that show up in severe thiamine deficiency: Thiamine deficiency
The classic Wernicke encephalopathy triad of ocular abnormalities, gait ataxia, and mental status changes is infrequently seen.
Remember the term "gait ataxia", it will come up again later. Moving on.
The first time was while I was on terbinafine in 2017 for a fungal infection.
The start of a problem is always a VERY important point.
Terbinafine is an anti-fungal medication that has a known reputation for being very hepatotoxic (toxic to the liver). The liver happens to be the main location of both Vitamin A storage and detoxification. Damage that, damage everything.
Here is my article about other antifungal medications that are known to inhibit the breakdown/detoxification of Vitamin A, eventually leading to chronic Vitamin A toxicity.
I need to connect something else very important here. You will want to read very carefully.
Some of any/all of the carotenoids, retinol, and retinyl esters you eat is eventually converted into 13-cis retinoic acid. This is not a debate, it is simply true.
13-cis retinoic is also sold to people in pharmaceutical pill form. It's called isotretinoin, or more familiarly, ACCUTANE. There is NO difference between the 13-cis retinoic acid that you take in an ACCUTANE pill and the 13-cis retinoic acid that your body turns carotenoids and retinoids into in your body. If you choose to argue, please take that to the chemists and biochemists who know much more about these things than internet armchair "Appeal to Nature" fallacy warriors, OK? They will tell you that there is NO difference. They cannot tell the difference between "natural" 13-cis retinoic acid and "synthetic" 13-cis retinoic acid in any bodily fluid. Therefore, they are the SAME.
Why is this important? Because terbinafine and 13-cis retinoic acid (isotretinoin) have a known drug-drug interaction that is extremely pertinent here!
I can't give a direct link on this one, so I'll tell you how to find it yourself, AND I'll give you a screenshot.
Go to https://www.drugbank.ca/drugs/DB00857, which is the entry for Terbinafine. Go to the section called "Drug Interactions". Enter "isotretinoin" in the search box in that section. It will give you this:
Let me repeat what the above says. Terbinafine + Isotretinoin (which is 13-cis retinoic acid) interact such that the risk or severity of myopathy [diseases of muscles], rhabdomyolysis, and myoglobinuria can be increased when Terbinafine is combined with Isotretinoin.
Therefore, because some portion of all the Vitamin A that a person consumes turns into 13-cis retinoic acid, it could be assumed that an excess of Vitamin A in the system would lead to an excess of 13-cis retinoic acid, and that 13-cis retinoic acid (aka Isotretinoin) could/would interact with the Terbinafine in the manner described above. Not good, right?
Keep the myopathy part in mind, I'll get back to it in just a couple lines.
The second was in January or so of this year after I’d switched my main carbs from beans and veggies to butternut squash.
It doesn't get any more obvious than this, folks.
Switching from beans and veggies to butternut squash (a type of winter squash) would drastically increase his Vitamin A intake. Just how high is butternut squash in Vitamin A? From Squash, winter:
The vivid orange flesh of many winter squash varieties is due to their amazing concentration of carotenoids. Among these carotenoids are beta-carotene, alpha-carotene, and other carotenoids that can be converted into active forms of vitamin A (retinoids). At WHFoods, winter squash actually makes its way into our Top 10 sources of vitamin A due to its carotenoid richness! In fact, among all 100 of our WHFoods, only sweet potato, carrot, and the green leafy vegetables surpass winter squash in terms of their total carotenoid content.
Top 10 sources of Vitamin A. A great way to get or worsen toxicity is to eat one of the foods highest in the toxin! Can one get Vitamin A toxic from food sources of carotenoids and retinoids? Yes, and remember when you read the below case study that pumpkin is a type of squash: Vitamin A toxicity secondary to excessive intake of yellow-green vegetables, liver and laver.
A 20-year-old Japanese woman had been eating pumpkin and only a very limited amount of other foods on a daily basis for 2 years. She was overly concerned about weight reduction. Aurantiasis cutis and abnormal liver function tests were noted by her family doctor in 1995 when she was 18 years old. At that time, she stopped eating pumpkin. However, she secretly continued an excessive intake of other beta-carotene-rich vegetables, liver and laver for about 2 years. Two and one-half years after being seen by her family physician, she experienced sudden onset of low-grade fever, limb edema, cheilitis, dry skin, and headache. These symptoms worsened daily. A liver needle biopsy was performed, and it showed a normal portal tract along with fat-laden Ito cells in the space of Disse. A final diagnosis of vitamin A poisoning and hepatic injury secondary to an eating disorder was made.
Please stop with the "food-based Vitamin A simply CAN'T become toxic!" trope. It's tired, delusional, and is not based in real science.
Now, one other thing. Regularly consuming beans is a solid approach to getting adequate dietary thiamine (but it doesn't work well for everyone's digestion). Remember how I talked about thiamine deficiency above?
The switch from "beans and veggies" to butternut squash did TWO things. It drastically INCREASED his Vitamin A intake, while drastically DECREASING his thiamine intake.
The gait problem came back. Note how I linked abnormal gait to both Vitamin A toxicity AND thiamine deficiency above.
There are NO coincidences.
This last time seemed to come up after I started tanning, which helps my eczema whenever it starts creeping up.
Is eczema a symptom of Vitamin A toxicity? Yes: Safety Assessment including Current and Emerging Issues in Toxicologic Pathology - Excess
The toxicity of Vitamin A (hypervitaminosis A) is manifested in two forms: acute and chronic.
[...]
Toxicity at the cellular level is manifested by redifferentiation of simple types of epithelium into more complex forms, including mucous epithelium. Accompanying this is decreased cohesion between epithelial cells in the skin. Accordingly, most affected humans report skin changes such as pruritis, erythema, eczema, and dermatitis, with bleeding and cracking of the skin, especially around lips and gums, as well as hair loss and nosebleeds.If one was Vitamin A toxic, this would mean that they have excess Vitamin A stored everywhere, including in the skin and subcutaneous fat. What happens when too much ultraviolet light is applied to the excess Vitamin A in the skin? It's not good: Photodecomposition of vitamin A and photobiological implications for the skin.
The biological effects of light-induced degradation of vitamin A and formation of reactive species are less understood and may be important for light-exposed tissues, such as the skin. Photochemical studies have demonstrated that excitation of retinol or its esters with UV light generates a number of reactive species including singlet oxygen and superoxide radical anion. These reactive oxygen species have been shown to damage a number of cellular targets, including lipids and DNA. Consistent with the potential for damaging DNA, retinyl palmitate has been shown to be photomutagenic in an in vitro test system. The results of mechanistic studies were consistent with mutagenesis through oxidative damage.
Apparently exposing Vitamin A to light (UV) creates all sorts of toxic, DNA-damaging (mutagenic) byproducts! I've written this whole article about how "sun poisoning" and "sun allergy" are simply the result of Vitamin A-toxic people getting too much sun for their toxic Vitamin A levels, and the sickness results from these toxic byproducts flooding the system afterwards.
Does light exposure do anything to deplete thiamine or other nutrients? Yes: Exposure to Sun Rays: An Investigation of Serum Micronutrient Status in Wistar Rats
Of all the micronutrients measured only thiamine, vitamin A, and pantothenic acid as well as minerals such as zinc, manganese and copper were
significantly lower in sun exposed rats compared with control.If sun exposure depletes thiamine, then it is likely that a tanning bed would too. Depleting zinc in a Vitamin A-toxic person would also be really bad, but I'm going to leave that part alone in order to keep this article from getting too big!
Am I surprised that Chris has eczema or had a bad reaction to (too much) tanning, based on what I know about all of this? Not at all.
The gait issue feels like I have to pick my legs up too high to move. My girlfriend noticed my left leg dragging too.
Remember myopathy from the Terbinafine + Isotretinoin part above? What is the primary symptom of myopathy? From the NINDS Myopathy Information Page:
The myopathies are neuromuscular disorders in which the primary symptom is muscle weakness due to dysfunction of muscle fiber.
Remember gait ataxia from above? What is that defined as? Ataxia from the Mayo Clinic:
Ataxia describes a lack of muscle control or coordination of voluntary movements, such as walking or picking up objects.
Is his "leg-lifting" problem due to weakness (myopathy) or lack of muscle control or coordination (ataxia)? We'll probably never know.
A bigger question is, when we know what the cause is and how to fix it, does figuring that out really matter at all? I say it doesn't.
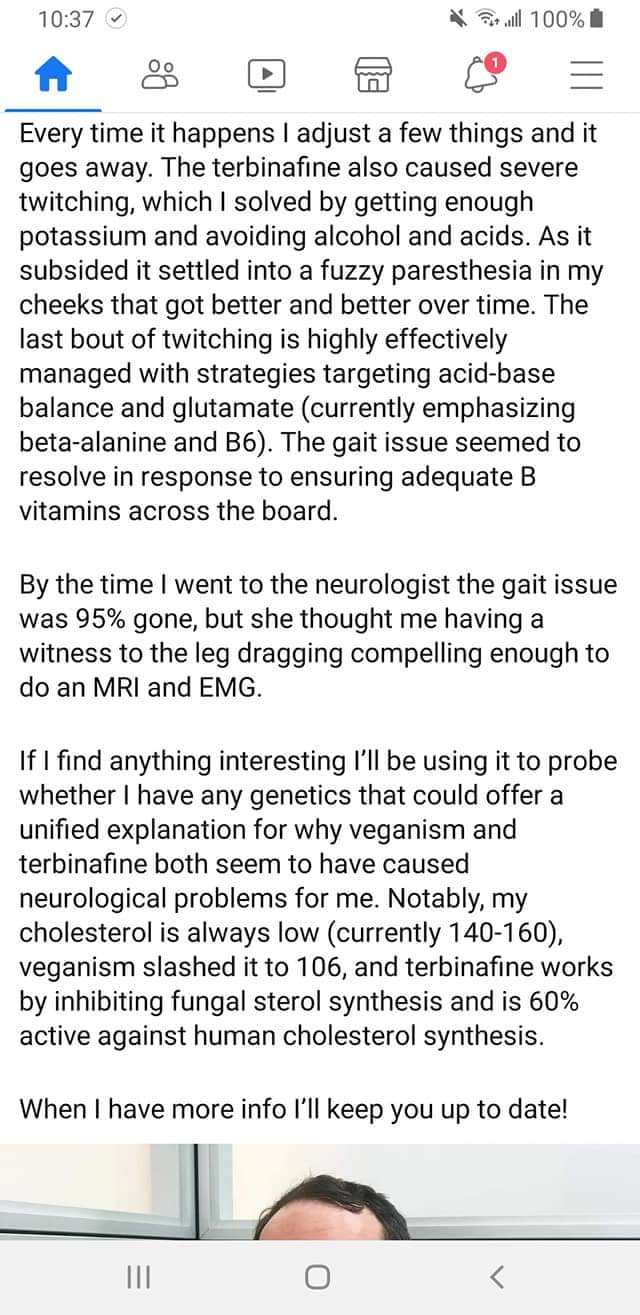
Every time it happens I adjust a few things and it goes away. The terbinafine also caused severe twitching, which I solved by getting enough potassium and avoiding alcohol and acids.
Here's an article I wrote about how Vitamin A BLOCKS potassium channels. Twitches can be related to a potassium deficiency. Blocked potassium channels would functionally look like a "deficiency", and the symptom could be reduced by getting more potassium. That does nothing to solve the root cause, however.
Is twitching related to thiamine deficiency? Let's see what his very own info page on thiamine says about it!
Thiamin, or vitamin B1, is central to both energy metabolism and antioxidant defense. While its deficiency causes many problems, out of all the B vitamins its deficiency is most neurological in nature, because energy metabolism of the brain becomes severely compromised, and because neurotransmitters derived from protein cannot be produced. In its most severe form, beriberi, it can cause loss of muscle control, twitching, muscles freezing into awkward positions, and seizures.
Loss of muscle control, like gait ataxia? Twitching? Interesting, right?
If you'll recall from above, ALCOHOL DEPLETES THIAMINE. Interesting that avoiding alcohol helped his symptoms, right?
What about alcohol and Vitamin A toxicity? Do those two things interact? Yes: Alcohol, vitamin A, and β-carotene: adverse interactions, including hepatotoxicity and carcinogenicity
It is, however, complicated by the intrinsic hepatotoxicity of retinol, which is potentiated by concomitant alcohol consumption. By contrast, β-carotene, a precursor of vitamin A, was considered innocuous until recently, when it was found to also interact with ethanol, which interferes with its conversion to retinol. Furthermore, the combination of β-carotene with ethanol results in hepatotoxicity.
Alcohol ENHANCES the toxicity of retinol and beta-carotene? It's almost like all these things are CONNECTED!
As it subsided it settled into a fuzzy paresthesia in my cheeks that got better and better over time.
Connecting paraesthesia (a burning or prickling sensation) and thiamine deficiency: Nutritional Neuropathies.
Clinical features of thiamine deficiency begin with distal sensory loss, burning pain, paraesthesias or muscle weakness in the toes and feet[6].
Hey, there's that muscle weakness (myopathy) part showing up again!
The last bout of twitching is highly effectively managed with strategies targeting acid-base balance and glutamate (currently emphasizing beta-alanine and B6).
"Managing" symptoms is not what I do. I am after the ROOT CAUSE.
The gait issue seemed to resolve in response to ensuring adequate B vitamins across the board.
"...seemed to resolve in response to ensuring adequate B-vitamins across the board". How was a nutrition guru's diet so deficient to begin with?
Let's cover the B-vitamins involved in several of the recurring themes here.
Avoiding alcohol relieves his symptoms, and alcohol seems to show up on his FB page regularly. What B-vitamin deficiencies have been associated in the research with the consumption of alcohol? The connections are clear.
Alcohol consumption is associated with lower thiamine (B1), pyridoxal 5-phosphate (B6), and folate (B9).
Alcohol consumption is associated with lower riboflavin (B2).
Alcohol consumption is associated with lower niacin (B3).
So we have now covered B1, B2, B3, B6, and B9. One big missing one is B12.
Remember how a part of any/all Vitamin A that one eats turns into 13-cis retinoic acid in the body (and is sold in pills as isotretinoin aka Accutane)? It has been demonstrated in multiple case studies that 13-cis retinoic acid (isotretinoin) is extremely effective at depleting cobalamin (B12) and folate (B9). We can then infer that Vitamin A toxicity would also deplete B12 and folate.
It needs to be said that alcohol (ethanol) and Vitamin A (retinol) use the EXACT same detox pathways (Alcohol dehydrogenase and Aldehyde dehydrogenase):
Ethanol —[Alcohol Dehydrogenase]→ Acetaldehyde —[Aldehyde Dehydrogenase]→ Acetic Acid
Retinol —[Alcohol Dehydrogenase]→ Retinaldehyde —[Aldehyde Dehydrogenase]→ Retinoic Acid
In some of the research, just to confuse people, the researchers switch the terms Alcohol Dehydrogenase for Retinol Dehydrogenase, and Aldehyde Dehydrogenase for Retinaldehyde Dehydrogenase. They all mean the same thing.
It is exceedingly likely that the nutrient deficiencies induced by alcohol also hold true for Vitamin A as well (the research isn't really looking for those though). This is likely why alcohol and Vitamin A are synergistically BAD (covered above)--because they induce the SAME nutrient deficiencies--and it would explain why the heroic effort at wide-spectrum B-vitamin supplementation is necessary to keep the symptoms at bay.
That covers the "B-vitamins across the board" issue well enough for me.
By the time I went to the neurologist the gait issue was 95% gone, but she thought me having a witness to the leg dragging compelling enough to do an MRI and EMG.
⠀
If I find anything interesting I’ll be using it to probe whether I have any genetics that could offer a unified explanation for why veganism and terbinafine both seem to have caused neurological problems for me.This is not a genetic problem. Not. At. All. It is a combination of toxicity and nutritional deficiency, as I have covered.
Why did veganism cause him such a problem?
Because veganism is a diet particularly suited to causing Vitamin A toxicity. Vegan diets are particularly prone to be excessive or deficient in the following things, any/all of which help lead the way to chronic Vitamin A toxicity:
- excessively high in carotenoids (he had a problem with butternut squash, remember)
- deficient in zinc
- completely lacking taurine (only found in meat protein, nowhere else)
- lacking total protein
- lacking total Calories
Notably, my cholesterol is always low (currently 140-160), veganism slashed it to 106, and terbinafine works by inhibiting fungal sterol synthesis and is 60% active against human cholesterol synthesis.
⠀
When I have more info I’ll keep you up to date!There's nothing to cover in that last bit above.
Back to the anxiety issue from the beginning of his post that I mentioned I would cover later.
Sure, anxiety in any medical situation is very normal. That said, when we look at the whole picture, other things arise.
Anxiety as a symptom of chronic Vitamin A toxicity: Vitamin A and Retinoids as Mitochondrial Toxicants
Really, a panoply of side effects has been observed that result from vitamin A intoxication that varies from acute intoxication including, for example, headache, hepatic swelling, vomiting, and diarrhea to chronic intoxication with induction of cognitive decline in subjects at different ages, as observed in the cases of increased irritability, confusion, anxiety disorders, depression, and suicide ideation [8, 9, 13]. The exact mechanism by which vitamin A and retinoids exert such effects is not clear yet. However, it may include cell cycle disarrangement, mitochondrial dysfunction, oxidative and nitrosative stress induction, and activation of cell death signaling in different experimental models.
Anxiety is also a symptom of thiamine (B1) deficiency.
Conclusion
To sum up, it is quite obvious to me that Chris has a severe and worsening chronic Vitamin A toxicity problem, severe B-vitamin (particularly thiamine) deficiency problems, and both of those issues are being exacerbated by continued alcohol consumption.
The clues are all there, the culprits have been identified.
If you like what you see, know that I take private clients from around the world for "Nutritional Restoration" based on testing, not guessing. I also have a private network at https://nutrition-restored.mn.co where my "Vitamin A, Aldehydes, and Glyphosate Detox" Program can be purchased for the do-it-yourself-ers.
First, I would like to make people aware that my intention is to help Chris so that he can potentially fix his numerous health issues, and if that is not possible, I'm hoping to help the other people who read this article and/or watch the video. While myself and others in the crowd who have fully realized the poison that is the non-"Vitamin" A, Chris has previously taken to ad hominem character attacks on us when we brought it up, calling us things like "flat earthers". He particularly didn't care for when I linked his aggressive FaceBook replies to this paper discussing aggression and chronic Vitamin A toxicity. Others noted that any discussion of chronic Vitamin A toxicity on his FaceBook page was quickly deleted. Oh well.
I am not digging into his health history any more than what he has put on the internet himself. This post that he put on FaceBook about his recent health issues and adventures in the conventional medical system is the one I will be discussing. I've heard from others about his internet-admitted past issues with exercise intolerance, heat intolerance, and allergies...all things that we regularly see improve on the Vitamin A Detox Program.
Just in case that post were to disappear, and for those who refuse to create FaceBook accounts (I admire you), here are screenshots of the post:

There is no good reason to downplay any of the signs and symptoms showing up in the above. He is far too young to be showing these significant neurological symptoms...unless he potentially was becoming toxic with something, and/or was severely deficient in something else. There is evidence and arguments for both, as you will see, and both go together.
In this article, I will lay out the science that shows that Chris has a severe and worsening chronic Vitamin A toxicity problem, severe B-vitamin (particularly thiamine) deficiency problems, and that both of those issues are being exacerbated by continued alcohol consumption.
I'm not going to re-post any of the post's associated pictures, as I think the words above are enough. I did note that in two of the three associated pictures he posted he was holding a beer, and in this post he talks about four drinks in one night while the picture is of yet another beer. I don't care how much someone drinks, I only care about how it affects the body-system and plays into the clues that his case left for me, the "Nutrition Detective". You'll see the reason for that term as we go through this piece by piece. Important things to keep in mind as we go on from this part are that alcohol has extremely negative interactions with Vitamin A, and that alcohol depletes thiamine (Vitamin B1). We will cover those more below.
Chris Masterjohn is well-known in nutritional circles as being a superfan of the Weston A. Price Foundation's (WAPF) general dietary guidelines of consuming MASSIVE amounts of Vitamin A from foods (liver, eggs, dairy, cod liver oil, squashes, etc.) and incorrectly believing that food-based Vitamin A is somehow magickally, completely, and utterly non-toxic. How wrong they are, and their followers (who often become my clients trying to fix the damage) and their children pay the price for it.
It should also be known that on his website he promotes discounts--and thus likely has financial arrangements with--at least two companies that sell organ meats in various forms. Why is this important? The old saying, "It is difficult to get a man to understand something, when his salary depends upon his not understanding it!" applies here.
Here are some of his articles over at the WAPF website showing an extreme pro-Vitamin A bias:
-
Vitamin A On Trial: Does Vitamin A Cause Osteoporosis?
- One can get a real feel for his position of downplaying chronic Vitamin A toxicity from the title of this section: How Much Vitamin A is Too Much? The Wrong Question to Ask [NOTE: asking how much is TOO MUCH is the MOST IMPORTANT question to ask!!!]
Who can forget the article & video he did about how he somehow got "Vitamin A deficient" in less than one month, which is IMPOSSIBLE for anyone to do! How do I know this? First, with his assumed/implied Vitamin A-heavy diet, he is nowhere near deficient in Vitamin A. Vitamin A is fat-soluble, which means it is stored in the liver and all over the body. Medscape says: "An adult liver can store up to a year's reserve of vitamin A." He absolutely did not "get deficient" in one month of eating a "low-Vitamin A" diet, certainly not when he regularly eats as many Vitamin A foods as he does! What likely happened is that his body started DETOXING/DUMPING that poison, causing him detoxification symptoms, because it FINALLY had the opportunity to do so!
PRO TIP: Read the comments of that article, where multiple people are asking him about their own Vitamin A toxicity problems!
What if we had insight into his diet, straight from Chris himself? We do, it is here: Why a Carnivore Diet is Problematic With Dr. Chris Masterjohn
I'm only going to include the pertinent Vitamin A toxicity-inducing portions below.
Excerpts from the section "Chris’ Guide To The Ideal Diet":
- Diversify your source of protein (meat, fish, poultry, shellfish, eggs, dairy, etc.)
- Diversity within the animal
- Make an effort to eat nose-to-tail
- Add 4-8 oz of liver to your diet each week
- Replace some meat with heart (if you’re feeling more adventurous, try kidney)
- Consume a large volume of vegetables
- Several cups per day
- Diversify across the colors (green, red, orange, yellow)
Every item I bolded above is a significant source of Vitamin A. I go over this more in the video. In combination, it is a recipe for excess, as you shall see.
Excerpts from the section "Chris' Masterjohn's Actual Diet"
- Modified due to digestive issues and not being able to absorb fructose well
- Chris’ typical meal:
- White rice
- A lot of mixed vegetables
- Meat or eggs
- A tomato product (usually salsa)
- 1 tbsp of unfortified nutritional yeast
- Chris will take oyster extract and liver supplements throughout the day
- His main fruit is bell pepper and tries to eat all colors
I'm going to spend a bit of time on this part. Again, every part I bolded is either high in Vitamin A or aggravates Vitamin A toxicity (again, I cover this more in the video).
Note the part about "not being able to metabolize fructose well." Research has shown in rats that Vitamin A toxicity slows down a key enzyme directly involved in FRUCTOSE metabolism: Early effects of hypervitaminosis A on gluconeogenic activity and amino acid metabolizing enzymes of rat liver.
Furthermore, hypervitaminosis A decreased the activities of two key hepatic glycolytic enzymes, phosphofructokinase, and pyruvate kinase, without affecting those of hexokinase and glucokinase.
Probably not a coincidence.
Liver pills and oyster extract are concentrated sources of Vitamin A.
Tomatoes and bell peppers, along with their inflammatory nightshade nature (you might recognize the author of that blog post 😉 ), are both very high in carotenoid Vitamin A.
Vegetables in the red, yellow, and orange color spectrums will always be high sources of Vitamin A.
Here's the kicker though. A study from the 1950s showed that rats that were given yeast or any fraction of liver (water-soluble OR fat-soluble) along with Vitamin A, got much worse symptoms of Vitamin A toxicity than rats that only got Vitamin A. It is also of note that tuna solubles, fish solubles, and acetone-extracted herring roe also worsened the Vitamin A toxicity problems...so the oyster extract potentially is looking similar in effect.
Chris says that this is his regular daily diet. Extremely high in Vitamin A, along with 2, maybe 3, other factors in it that have been shown to worsen Vitamin A toxicity symptoms.
Now, let's go into his FB post. The quotes are from his post, my comments are in between.
I went in for an MRI last night. I was nervous AF about getting injected with gadolinium contrast and you can probably tell the anxiety level is way higher in my before picture versus in the post-MRI beer pic.
I want to get to the bigger things first. I re-visit the anxiety below, after painting the bigger picture first.
I’m investigating an abnormal gait that has crept up on me three times now.
A recurring/repeating issue could easily imply that either a toxicity state keeps returning, or a deficiency state keeps returning, or both. One should be able to figure out that if it is recurring, the root cause of the problem has NOT been dealt with. It has only been symptomatically addressed.
Is "abnormal gait" a symptom of chronic Vitamin A toxicity? Yes, and across multiple species.
In cats: Skeletal Abnormalities in the Hindlimbs of Young Cats as a result of Hypervitaminosis A
HYPERVITAMINOSIS A causes extensive confluent exostosis formation of the cervical spine in adult cats1,2. It was initially reported that no juvenile osteodystrophy occurred in this disease1, but an abnormal hindquarter gait was described later in a group of young cats receiving large daily doses of vitamin A (ref. 2). No explanation of this abnormal gait was given and the condition was therefore studied further.
Add in pigs and humans: Hypervitaminosis A in the pig.
Premature cIosure of epiphyseal cartilages and changes in the structure of epiphyses themselves, gave rise to joints of abnormal structure, direction and amplitude of movement leading to lameness and gait changes. This has been amply demonstrated in experimental hypervitaminosis A of young cats (Clark and Seawright 1968) and also in children recovering from hypervitaminosis A (Pease 1962).
"...amply demonstrated..." I think that is strong enough wording from a 50-year-old paper for my purposes here.
Now, let's move on to thiamine. Has thiamine deficiency ever been associated with "abnormal gait"? Yes. So much so that there's a specific name for the neurological triad of disease symptoms that show up in severe thiamine deficiency: Thiamine deficiency
The classic Wernicke encephalopathy triad of ocular abnormalities, gait ataxia, and mental status changes is infrequently seen.
Remember the term "gait ataxia", it will come up again later. Moving on.
The first time was while I was on terbinafine in 2017 for a fungal infection.
The start of a problem is always a VERY important point.
Terbinafine is an anti-fungal medication that has a known reputation for being very hepatotoxic (toxic to the liver). The liver happens to be the main location of both Vitamin A storage and detoxification. Damage that, damage everything.
Here is my article about other antifungal medications that are known to inhibit the breakdown/detoxification of Vitamin A, eventually leading to chronic Vitamin A toxicity.
I need to connect something else very important here. You will want to read very carefully.
Some of any/all of the carotenoids, retinol, and retinyl esters you eat is eventually converted into 13-cis retinoic acid. This is not a debate, it is simply true.
13-cis retinoic is also sold to people in pharmaceutical pill form. It's called isotretinoin, or more familiarly, ACCUTANE. There is NO difference between the 13-cis retinoic acid that you take in an ACCUTANE pill and the 13-cis retinoic acid that your body turns carotenoids and retinoids into in your body. If you choose to argue, please take that to the chemists and biochemists who know much more about these things than internet armchair "Appeal to Nature" fallacy warriors, OK? They will tell you that there is NO difference. They cannot tell the difference between "natural" 13-cis retinoic acid and "synthetic" 13-cis retinoic acid in any bodily fluid. Therefore, they are the SAME.
Why is this important? Because terbinafine and 13-cis retinoic acid (isotretinoin) have a known drug-drug interaction that is extremely pertinent here!
I can't give a direct link on this one, so I'll tell you how to find it yourself, AND I'll give you a screenshot.
Go to https://www.drugbank.ca/drugs/DB00857, which is the entry for Terbinafine. Go to the section called "Drug Interactions". Enter "isotretinoin" in the search box in that section. It will give you this:
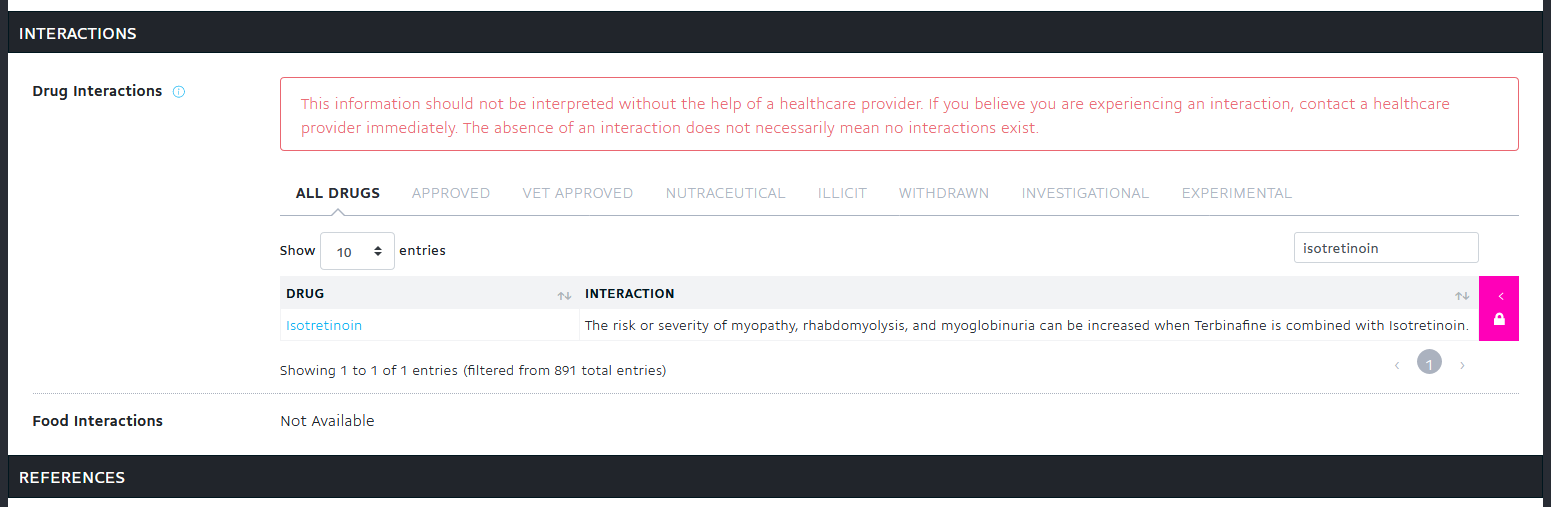
Let me repeat what the above says. Terbinafine + Isotretinoin (which is 13-cis retinoic acid) interact such that the risk or severity of myopathy [diseases of muscles], rhabdomyolysis, and myoglobinuria can be increased when Terbinafine is combined with Isotretinoin.
Therefore, because some portion of all the Vitamin A that a person consumes turns into 13-cis retinoic acid, it could be assumed that an excess of Vitamin A in the system would lead to an excess of 13-cis retinoic acid, and that 13-cis retinoic acid (aka Isotretinoin) could/would interact with the Terbinafine in the manner described above. Not good, right?
Keep the myopathy part in mind, I'll get back to it in just a couple lines.
The second was in January or so of this year after I’d switched my main carbs from beans and veggies to butternut squash.
It doesn't get any more obvious than this, folks.
Switching from beans and veggies to butternut squash (a type of winter squash) would drastically increase his Vitamin A intake. Just how high is butternut squash in Vitamin A? From Squash, winter:
The vivid orange flesh of many winter squash varieties is due to their amazing concentration of carotenoids. Among these carotenoids are beta-carotene, alpha-carotene, and other carotenoids that can be converted into active forms of vitamin A (retinoids). At WHFoods, winter squash actually makes its way into our Top 10 sources of vitamin A due to its carotenoid richness! In fact, among all 100 of our WHFoods, only sweet potato, carrot, and the green leafy vegetables surpass winter squash in terms of their total carotenoid content.
Top 10 sources of Vitamin A. A great way to get or worsen toxicity is to eat one of the foods highest in the toxin! Can one get Vitamin A toxic from food sources of carotenoids and retinoids? Yes, and remember when you read the below case study that pumpkin is a type of squash: Vitamin A toxicity secondary to excessive intake of yellow-green vegetables, liver and laver.
A 20-year-old Japanese woman had been eating pumpkin and only a very limited amount of other foods on a daily basis for 2 years. She was overly concerned about weight reduction. Aurantiasis cutis and abnormal liver function tests were noted by her family doctor in 1995 when she was 18 years old. At that time, she stopped eating pumpkin. However, she secretly continued an excessive intake of other beta-carotene-rich vegetables, liver and laver for about 2 years. Two and one-half years after being seen by her family physician, she experienced sudden onset of low-grade fever, limb edema, cheilitis, dry skin, and headache. These symptoms worsened daily. A liver needle biopsy was performed, and it showed a normal portal tract along with fat-laden Ito cells in the space of Disse. A final diagnosis of vitamin A poisoning and hepatic injury secondary to an eating disorder was made.
Please stop with the "food-based Vitamin A simply CAN'T become toxic!" trope. It's tired, delusional, and is not based in real science.
Now, one other thing. Regularly consuming beans is a solid approach to getting adequate dietary thiamine (but it doesn't work well for everyone's digestion). Remember how I talked about thiamine deficiency above?
The switch from "beans and veggies" to butternut squash did TWO things. It drastically INCREASED his Vitamin A intake, while drastically DECREASING his thiamine intake.
The gait problem came back. Note how I linked abnormal gait to both Vitamin A toxicity AND thiamine deficiency above.
There are NO coincidences.
This last time seemed to come up after I started tanning, which helps my eczema whenever it starts creeping up.
Is eczema a symptom of Vitamin A toxicity? Yes: Safety Assessment including Current and Emerging Issues in Toxicologic Pathology - Excess
The toxicity of Vitamin A (hypervitaminosis A) is manifested in two forms: acute and chronic.
[...]
Toxicity at the cellular level is manifested by redifferentiation of simple types of epithelium into more complex forms, including mucous epithelium. Accompanying this is decreased cohesion between epithelial cells in the skin. Accordingly, most affected humans report skin changes such as pruritis, erythema, eczema, and dermatitis, with bleeding and cracking of the skin, especially around lips and gums, as well as hair loss and nosebleeds.
If one was Vitamin A toxic, this would mean that they have excess Vitamin A stored everywhere, including in the skin and subcutaneous fat. What happens when too much ultraviolet light is applied to the excess Vitamin A in the skin? It's not good: Photodecomposition of vitamin A and photobiological implications for the skin.
The biological effects of light-induced degradation of vitamin A and formation of reactive species are less understood and may be important for light-exposed tissues, such as the skin. Photochemical studies have demonstrated that excitation of retinol or its esters with UV light generates a number of reactive species including singlet oxygen and superoxide radical anion. These reactive oxygen species have been shown to damage a number of cellular targets, including lipids and DNA. Consistent with the potential for damaging DNA, retinyl palmitate has been shown to be photomutagenic in an in vitro test system. The results of mechanistic studies were consistent with mutagenesis through oxidative damage.
Apparently exposing Vitamin A to light (UV) creates all sorts of toxic, DNA-damaging (mutagenic) byproducts! I've written this whole article about how "sun poisoning" and "sun allergy" are simply the result of Vitamin A-toxic people getting too much sun for their toxic Vitamin A levels, and the sickness results from these toxic byproducts flooding the system afterwards.
Does light exposure do anything to deplete thiamine or other nutrients? Yes: Exposure to Sun Rays: An Investigation of Serum Micronutrient Status in Wistar Rats
Of all the micronutrients measured only thiamine, vitamin A, and pantothenic acid as well as minerals such as zinc, manganese and copper were
significantly lower in sun exposed rats compared with control.
If sun exposure depletes thiamine, then it is likely that a tanning bed would too. Depleting zinc in a Vitamin A-toxic person would also be really bad, but I'm going to leave that part alone in order to keep this article from getting too big!
Am I surprised that Chris has eczema or had a bad reaction to (too much) tanning, based on what I know about all of this? Not at all.
The gait issue feels like I have to pick my legs up too high to move. My girlfriend noticed my left leg dragging too.
Remember myopathy from the Terbinafine + Isotretinoin part above? What is the primary symptom of myopathy? From the NINDS Myopathy Information Page:
The myopathies are neuromuscular disorders in which the primary symptom is muscle weakness due to dysfunction of muscle fiber.
Remember gait ataxia from above? What is that defined as? Ataxia from the Mayo Clinic:
Ataxia describes a lack of muscle control or coordination of voluntary movements, such as walking or picking up objects.
Is his "leg-lifting" problem due to weakness (myopathy) or lack of muscle control or coordination (ataxia)? We'll probably never know.
A bigger question is, when we know what the cause is and how to fix it, does figuring that out really matter at all? I say it doesn't.
Every time it happens I adjust a few things and it goes away. The terbinafine also caused severe twitching, which I solved by getting enough potassium and avoiding alcohol and acids.
Here's an article I wrote about how Vitamin A BLOCKS potassium channels. Twitches can be related to a potassium deficiency. Blocked potassium channels would functionally look like a "deficiency", and the symptom could be reduced by getting more potassium. That does nothing to solve the root cause, however.
Is twitching related to thiamine deficiency? Let's see what his very own info page on thiamine says about it!
Thiamin, or vitamin B1, is central to both energy metabolism and antioxidant defense. While its deficiency causes many problems, out of all the B vitamins its deficiency is most neurological in nature, because energy metabolism of the brain becomes severely compromised, and because neurotransmitters derived from protein cannot be produced. In its most severe form, beriberi, it can cause loss of muscle control, twitching, muscles freezing into awkward positions, and seizures.
Loss of muscle control, like gait ataxia? Twitching? Interesting, right?
If you'll recall from above, ALCOHOL DEPLETES THIAMINE. Interesting that avoiding alcohol helped his symptoms, right?
What about alcohol and Vitamin A toxicity? Do those two things interact? Yes: Alcohol, vitamin A, and β-carotene: adverse interactions, including hepatotoxicity and carcinogenicity
It is, however, complicated by the intrinsic hepatotoxicity of retinol, which is potentiated by concomitant alcohol consumption. By contrast, β-carotene, a precursor of vitamin A, was considered innocuous until recently, when it was found to also interact with ethanol, which interferes with its conversion to retinol. Furthermore, the combination of β-carotene with ethanol results in hepatotoxicity.
Alcohol ENHANCES the toxicity of retinol and beta-carotene? It's almost like all these things are CONNECTED!
As it subsided it settled into a fuzzy paresthesia in my cheeks that got better and better over time.
Connecting paraesthesia (a burning or prickling sensation) and thiamine deficiency: Nutritional Neuropathies.
Clinical features of thiamine deficiency begin with distal sensory loss, burning pain, paraesthesias or muscle weakness in the toes and feet[6].
Hey, there's that muscle weakness (myopathy) part showing up again!
The last bout of twitching is highly effectively managed with strategies targeting acid-base balance and glutamate (currently emphasizing beta-alanine and B6).
"Managing" symptoms is not what I do. I am after the ROOT CAUSE.
The gait issue seemed to resolve in response to ensuring adequate B vitamins across the board.
"...seemed to resolve in response to ensuring adequate B-vitamins across the board". How was a nutrition guru's diet so deficient to begin with?
Let's cover the B-vitamins involved in several of the recurring themes here.
Avoiding alcohol relieves his symptoms, and alcohol seems to show up on his FB page regularly. What B-vitamin deficiencies have been associated in the research with the consumption of alcohol? The connections are clear.
Alcohol consumption is associated with lower thiamine (B1), pyridoxal 5-phosphate (B6), and folate (B9).
Alcohol consumption is associated with lower riboflavin (B2).
Alcohol consumption is associated with lower niacin (B3).
So we have now covered B1, B2, B3, B6, and B9. One big missing one is B12.
Remember how a part of any/all Vitamin A that one eats turns into 13-cis retinoic acid in the body (and is sold in pills as isotretinoin aka Accutane)? It has been demonstrated in multiple case studies that 13-cis retinoic acid (isotretinoin) is extremely effective at depleting cobalamin (B12) and folate (B9). We can then infer that Vitamin A toxicity would also deplete B12 and folate.
It needs to be said that alcohol (ethanol) and Vitamin A (retinol) use the EXACT same detox pathways (Alcohol dehydrogenase and Aldehyde dehydrogenase):
Ethanol —[Alcohol Dehydrogenase]→ Acetaldehyde —[Aldehyde Dehydrogenase]→ Acetic Acid
Retinol —[Alcohol Dehydrogenase]→ Retinaldehyde —[Aldehyde Dehydrogenase]→ Retinoic Acid
In some of the research, just to confuse people, the researchers switch the terms Alcohol Dehydrogenase for Retinol Dehydrogenase, and Aldehyde Dehydrogenase for Retinaldehyde Dehydrogenase. They all mean the same thing.
It is exceedingly likely that the nutrient deficiencies induced by alcohol also hold true for Vitamin A as well (the research isn't really looking for those though). This is likely why alcohol and Vitamin A are synergistically BAD (covered above)--because they induce the SAME nutrient deficiencies--and it would explain why the heroic effort at wide-spectrum B-vitamin supplementation is necessary to keep the symptoms at bay.
That covers the "B-vitamins across the board" issue well enough for me.
By the time I went to the neurologist the gait issue was 95% gone, but she thought me having a witness to the leg dragging compelling enough to do an MRI and EMG.
⠀
If I find anything interesting I’ll be using it to probe whether I have any genetics that could offer a unified explanation for why veganism and terbinafine both seem to have caused neurological problems for me.
This is not a genetic problem. Not. At. All. It is a combination of toxicity and nutritional deficiency, as I have covered.
Why did veganism cause him such a problem?
Because veganism is a diet particularly suited to causing Vitamin A toxicity. Vegan diets are particularly prone to be excessive or deficient in the following things, any/all of which help lead the way to chronic Vitamin A toxicity:
- excessively high in carotenoids (he had a problem with butternut squash, remember)
- deficient in zinc
- completely lacking taurine (only found in meat protein, nowhere else)
- lacking total protein
- lacking total Calories
Notably, my cholesterol is always low (currently 140-160), veganism slashed it to 106, and terbinafine works by inhibiting fungal sterol synthesis and is 60% active against human cholesterol synthesis.
⠀
When I have more info I’ll keep you up to date!
There's nothing to cover in that last bit above.
Back to the anxiety issue from the beginning of his post that I mentioned I would cover later.
Sure, anxiety in any medical situation is very normal. That said, when we look at the whole picture, other things arise.
Anxiety as a symptom of chronic Vitamin A toxicity: Vitamin A and Retinoids as Mitochondrial Toxicants
Really, a panoply of side effects has been observed that result from vitamin A intoxication that varies from acute intoxication including, for example, headache, hepatic swelling, vomiting, and diarrhea to chronic intoxication with induction of cognitive decline in subjects at different ages, as observed in the cases of increased irritability, confusion, anxiety disorders, depression, and suicide ideation [8, 9, 13]. The exact mechanism by which vitamin A and retinoids exert such effects is not clear yet. However, it may include cell cycle disarrangement, mitochondrial dysfunction, oxidative and nitrosative stress induction, and activation of cell death signaling in different experimental models.
Anxiety is also a symptom of thiamine (B1) deficiency.
Conclusion
To sum up, it is quite obvious to me that Chris has a severe and worsening chronic Vitamin A toxicity problem, severe B-vitamin (particularly thiamine) deficiency problems, and both of those issues are being exacerbated by continued alcohol consumption.
The clues are all there, the culprits have been identified.
If you like what you see, know that I take private clients from around the world for "Nutritional Restoration" based on testing, not guessing. I also have a private network at https://nutrition-restored.mn.co where my "Vitamin A, Aldehydes, and Glyphosate Detox" Program can be purchased for the do-it-yourself-ers.
Licensed Naturopathic Physician (NMD) in Arizona
NutritionDetective.com, home of the Love Your Liver program
YouTube - FaceBook - Instagram - Twitter
